Terms of use
1. GENERAL TERMS AND CONDITIONS
Thank you for visiting the Evidencio website/app (the "Site" or "website"). Please read the Terms and Conditions contained in this document carefully since any use of this site constitutes your acceptance of the Terms and Conditions set out herein. If you do not agree to these terms and conditions, you may not use this website.
Throughout this site, the terms "we", "us", "our" and "Evidencio" refer to Evidencio BV, and any of its direct and indirect subsidiaries. "You" refers to any person accessing and/or using this website.
1.1 USE
In order to use the Site you must be at least 18 years old. If you are not at least 18 years old you may not use this Site.
Evidencio hereby gives You a personal, non-exclusive, non-transferable, free of charge right to access and use the Site (without any right of sub-license).
You undertake to and agree with Evidencio that You will:
- not use the Site for or on behalf of any third party or to provide a service, except as may be expressly permitted by a separate subscription or license agreement between Evidencio and Yourself or an Organization you legally represent;
- limit Your use of the Site to Your own personal, internal academic or other non-commercial use, except as may be expressly permitted by a separate subscription or license agreement between Evidencio and Yourself or an Organization you legally represent;
- use the Site in accordance with the prevailing instructions and guidance for use given on the Site and faithfully comply with our procedures for user identification, authentication and access;
- comply with all applicable laws and regulations with respect to Your use of the Site; and
- except to the extent expressly permitted under this agreement, not attempt to: reverse compile, disassemble, reverse engineer or copy, modify, duplicate, create derivative works from, frame, mirror, republish, download, display, transmit, or distribute all or any portion of the Site in any form or media or by any means.
- accept our Disclaimer
Evidencio may at its own discretion offer varying features, functionalities and services, limit usage quotas, or impose particular usage conditions to/for users identified as, for example "anonymous users", "registered users", "subscription users", and "API-users".
1.2 CHANGES
We reserve the right to change, modify, add or remove these Terms and Conditions at any time, and you agree (including by virtue of your continued use of our site) to be bound by any such changes. Unless explicitly stated otherwise, any new features or functionality (including, without limitation, video and related projects) that augment or enhance our site shall be subject to these Terms and Conditions. Please check these Terms and Conditions periodically for any modifications. The most current version of these Terms of Use can be viewed at any time at: https://www.evidencio.com/terms-conditions.
1.3 LINKS
The Site may contain links to third-party sites or resources. Evidencio is not responsible for the availability of external sites or resources linked to the Site, and does not endorse and is not responsible or liable for any content, advertising, products or other materials on or available from such sites or resources. Transactions that occur between you and any third party are strictly between you and the third party and are not the responsibility of Evidencio. Because we are not responsible for the availability or accuracy of these outside resources or their contents, you should review the terms and conditions and privacy policies of these linked sites, as their policies may differ from ours.
We welcome links to the Site. You may establish a hypertext link to the Site, provided that the link does not state or imply any sponsorship or endorsement of your site by Evidencio. We grant a nonexclusive, limited permission ("Permission") to display the Trademarks contained in Evidencio domain names, brand names and logos to the owner(s) of any web sites ("Owner") that would like to develop a link between their site and the corresponding website owned by Evidencio ("Evidencio Site"). Links to an Evidencio Site other than the one using the Evidencio domain names, brand names or logos are not permitted. The materials on the Owner's site shall not imply any association with or relation to Evidencio or imply in any way that any materials from our Evidencio Site are maintained within Owner's web site.
No changes or modifications to the Evidencio domain names, brand names or logos may be made. Use of the Evidencio domain names, brand names or logos for purposes other than linking to the Evidencio Site is expressly forbidden. The domain names, brand names and logos must not be used or associated with any obscene, scandalous, inflammatory, pornographic, indecent, profane, defamatory or unlawful site or materials in any way, or in any manner that would adversely affect the name, reputation and goodwill of Evidencio and its products. We retain and reserve all rights in and to Evidencio's trade names, trademarks, copyrights and all other intellectual property with respect to its domain names, brand names and logos. Evidencio reserves the right to cancel the Permission at any time and for any reason. Upon receipt of such notification, use of the domain names, brand names or logos must cease and the link between the web sites must terminate. Use of Evidencio trademarks, trade names, logos, copyrighted material or any other intellectual property of Evidencio for any purpose not stated herein is expressly forbidden.
1.4 LEGALLY-COMPELLED DISCLOSURE OF USER INFORMATION
You agree that in the event we receive a subpoena issued by a court or from a law enforcement or government agency, we shall comply with such subpoenas without your consent or prior notice to you and may disclose your IP address, username, name, IP location or other information in response thereto.
1.5 SYSTEMS RELIABILITY
Evidencio aims to keep the Site available twenty-four (24) hours a day, seven (7) days a week and to maintain saved information. However, Evidencio shall not be liable for any lost, altered, or corrupted information or any damages related to non-availability of the Site.
1.6 PROHIBITED ACTIVITIES
You are prohibited from doing any act that Evidencio in its absolute discretion may deem to be inappropriate and/or would be deemed to be an unlawful act or is prohibited by any laws applicable to this website including but not limited to:
- Any act that would constitute a breach of either the privacy (including uploading private information without the concerned individual's consent) or any other of the legal rights of individuals
- Using this website to defame or libel Evidencio, its employees or other individuals or acting in such a way that brings into disrepute the good name of Evidencio;
- Uploading files that contain viruses that may cause damage to the property of Evidencio or the property of other individuals; and
- Posting or transmitting to this website any non-authorized material including but not limited to material that is in our opinion likely to cause annoyance, detrimental to or in violation of Evidencio's or any third party's systems or network security, libelous, defamatory, racist, obscene, threatening, pornographic, profane or is otherwise unlawful.
1.7 DISCLAIMER OF WARRANTIES AND LIABILITY
Unless explicitly agreed upon otherwise, e.g. as part of a paid Evidencio Subscription agreement:
- Neither Evidencio nor its suppliers or licensors makes any warranty whatsoever, including without limitation, that the operation of the Site will be uninterrupted or error-free; that any defects will be corrected; that the Site, including the server that makes it available, is free of viruses or other harmful components; or as to the accuracy, completeness, reliability, availability, suitability, quality, non-infringement, operation or result obtained from the use of any Content, product or service provided on, accessible from or distributed through the Site.
- THE SITE AND ALL CONTENT, PRODUCTS AND SERVICES INCLUDED IN OR ACCESSIBLE FROM THE SITE ARE PROVIDED "AS IS" AND WITHOUT WARRANTIES OR REPRESENTATIONS OF ANY KIND (EXPRESS, IMPLIED AND STATUTORY, INCLUDING BUT NOT LIMITED TO THE WARRANTIES OF TITLE AND NONINFRINGEMENT AND THE IMPLIED WARRANTIES OF MERCHANTABILITY AND FITNESS FOR A PARTICULAR PURPOSE), ALL OF WHICH EVIDENCIO DISCLAIMS TO THE FULLEST EXTENT PERMITTED BY LAW. YOUR USE OF THE SITE AND ITS CONTENT, PRODUCTS AND SERVICES IS AT YOUR SOLE RISK.
- To the extent permitted under applicable law, no responsibility is assumed for any injury and/or damage to persons, animals or property as a matter of products liability, negligence or otherwise, or from any use or operation of any ideas, instructions, methods, products or procedures contained in the Site. Medical and healthcare providers should exercise their own independent clinical judgment. No suggested test or procedure should be carried out unless, in the provider's judgment, its use is justified. Because of rapid advances in the medical sciences, we recommend that the independent verification of diagnoses, indications and drug dosages should be made. Discussions, views, and recommendations as to medical or health care procedures, methods, products, choice of drugs, and drug dosages are the responsibility of the authors.
- TO THE EXTENT PERMITTED UNDER APPLICABLE LAW, IN NO EVENT SHALL EVIDENCIO OR ITS SUPPLIERS OR LICENSORS BE LIABLE FOR ANY DAMAGES (INCLUDING, WITHOUT LIMITATION, CONSEQUENTIAL, SPECIAL, INCIDENTAL, INDIRECT, OR SIMILAR DAMAGES, PERSONAL INJURY (INCLUDING DEATH), LOSS OF PROFITS, CORRUPTION OR LOSS OF DATA, BUSINESS INTERRUPTION OR ANY OTHER COMMERCIAL DAMAGES OR LOSSES) ARISING OUT OF OR IN CONNECTION WITH THE USE OR PERFORMANCE OF THE SITE OR ITS CONTENT, PRODUCTS OR SERVICES, OR SHALL THE LIABILITY OF EVIDENCIO OR ITS SUPPLIERS AND LICENSORS EXCEED A SUM EQUAL TO THE FEES PAID BY YOU HEREUNDER, EVEN IF ADVISED OF THE POSSIBILITY OF SUCH DAMAGES.
- Evidencio does not claim ownership, endorse or take responsibility for any third-party products, information, guidelines, materials or services that may be offered, advertised, provided or displayed on the Site or incorporated in the Content, products or services contained on, accessible from or distributed through the Site.
- Regarding the use of algorithms, calculators, algorithms and other tools provided by Evidencio our website or as part of our services our Legal Disclaimer applies
1.8 EXPORT RESTRICTIONS
Software from this Site may be further subject to Export laws, rules and regulations, as amended from time to time.
1.9 MOBILE SERVICES
If Evidencio permits or makes available to you the ability to: (a) upload content to the website via your mobile telephone and/or tablet ("mobile device"), (b) receive and reply to messages, or to access or make posts using text messaging, (c) browse the site from your mobile device or (d) to access features through a mobile application you have downloaded and installed on your mobile device (collectively "Mobile Services"), your mobile carrier's standard data, Internet, messaging and other service fees and charges apply to your use of, and access to, the Mobile Services, and you are solely responsible for all such fees and charges. The Mobile Services may not be compatible with all mobile devices, carriers, and services, and Evidencio does not make any representations or warranties regarding such compatibility. You are solely responsible for ensuring that your mobile device is compatible with the type of content being provided through the Mobile Services. You understand that content delivered as part of the Mobile Services may be delivered to your device through premium mobile services and acknowledge that you are solely and exclusively responsible for any charges for such services, including but not limited to any roaming charges.
You may be given the option to register to receive commercial messages from Evidencio via your mobile device. You understand that you may be charged by your wireless service provider in connection with the receipt of such messages. You may "opt out" of receiving future messages by following the instructions provided (i) in the wireless messages or (ii) on the website where you registered to receive such messages.
1.10 JURISDICTION AND GOVERNING LAW
The Evidencio products, services, materials, offers and information appearing on this Site are intended for users and/or customers worldwide. However Evidencio makes no representation that the products, services, and content of this website are appropriate or available in locations other than the Netherlands.
You and Evidencio agree that any controversy or claim arising from or pertaining to the use of this website shall be governed by the laws of the Netherlands, without giving effect to any choice-of-law provisions, and be submitted to the exclusive jurisdiction of the courts of the Netherlands.
2. USER CONTENT SUBMISSION GUIDELINES
We may allow you to comment on and participate in interactive features on our Site, e.g. our comments section, or in social communities owned by Evidencio. We may also allow you to submit content and materials for use on our Site via our online forms and features. For example, as a creator/editor of a calculator, formula or equation you may be able to submit text, calculation logic, code, photographs, messages, or videos. The things you post or submit for use on our Site are "User Content".
You agree to these submission guidelines ("Guidelines"), our full Terms and Conditions and any additional terms by submitting User Content.
2.1 ALL USER CONTENT SUBMITTED TO US
You agree that your User Content is accurate and complete. You also agree that:
- Your User Content is created exclusively by you. This means that you did not copy it from any other source. If you did not create your User Content, anyone that created it or helped create it must give you permission to submit your User Content to us. You must obtain consent and a release from any person (or the legal guardians of any persons) depicted in your User Content before you submit it with full knowledge from these persons that we may exploit it in any manner whatsoever. Anyone you get consent from must understand that we will use the content you submit in any manner we think is appropriate.
- Your User Content does not threaten or disparage others. This includes not harassing or intimidating other users. It also includes not defaming or libeling anyone. Your User Content does not use hateful language. This includes not making negative comments connected to race, national origin or religion. You also cannot disparage someone because of their gender, age, or sexual preference.
- Your User Content does not disclose confidential or personal information about others. Your User Content will only disclose personal information with the other person's consent. This also means that your User Content does not include information you must keep confidential under contract. This also means that your User Content does not violate anyone's privacy or publicity rights.
2.2 USER CONTENT SUBMITTED FOR USE ON OUR SITE
- You agree that any material you submit to our page by upload, or otherwise, including any data, questions, comments, ideas, suggestions or the like ("Site Content") are, and will be treated as, non-confidential and non-proprietary.
- You grant us an unrestricted, royalty-free license to your submitted Site Content. We may use your Site Content in any manner, including hosting, caching, copying, selling, or distributing your Site Content. You also understand that we may modify, edit, reformat, or translate your Site Content.
- We may use and publish your Site Content in any format and in all media that exists now, or may exist in the future. You agree that we may use any part of your Site Content, including any of your ideas, concepts, or techniques for any purpose, and that any such use is without compensation to you. For example, we may use your Site Content to develop, manufacture and market products. We may sub-license any of these rights to other third parties. These third parties may benefit from the rights and licenses granted to us under these Submission Guidelines, our Terms of Use and any Additional Terms. Your Site Content may be searched and accessed by others.
- You represent and warrant that you own your Site Content and have the right to grant the license described above. You further represent and warrant that our use of your Site Content will not violate anyone's intellectual property rights or other rights of any person or entity or otherwise place us in breach of any applicable laws. Evidencio is under no obligation to use the information submitted. You understand that Evidencio employs both internal and external resources which may have developed or may in the future develop ideas identical or similar to your Site Content and that Evidencio is only willing to consider the submissions of Site Content on these terms.
2.3 USER CONTENT SUBMITTED FOR USE ON OUR SITE AS LICENSED CONTENT
- You grant us a restricted, royalty-bearing license to your submitted Site Content. We may use your licensed Site Content as part of paid services and subscriptions offered to other Evidencio users or third parties. You also understand that we may modify, edit, reformat, or translate your Site Content.
- We may use and publish your Site Content in any format and in all media that exists now, or may exist in the future as part of paid subscriptions and services offered by Evidencio. You agree that we may use any part of your Site Content, and that any such use is subject only to the applicable compensation to you as defined by our current pricing and licensing plans.
- We may use your Site Content to develop, manufacture and market products. We may sub-license any of these rights to other third parties. These third parties may benefit from the rights and licenses granted to us under these Submission Guidelines, our Terms of Use and any Additional Terms. Your Site Content may be searched and accessed by others.
- You represent and warrant that you own your Site Content and have the right to grant the license described above. You further represent and warrant that our use of your Site Content will not violate anyone's intellectual property rights or other rights of any person or entity or otherwise place us in breach of any applicable laws. Evidencio is under no obligation to use the information submitted. You understand that Evidencio employs both internal and external resources which may have developed or may in the future develop ideas identical or similar to your Site Content and that Evidencio is only willing to consider the submissions of Site Content on these terms.
2.4 USER CONTENT POSTED ON OUR COMMUNITIES
Our social media pages ("Communities") are for expressing opinions and creating discussions. We allow postings ("Community Content") on these pages following these guidelines. We ask that you play nice and be polite. While we encourage the sharing of your comments, photos, videos, and links, please understand that the Community Content posted to our Communities does not represent the opinions of Evidencio or its affiliates. Community Content that we feel are offensive, inappropriate or not otherwise keeping with the spirit of the page, such as advertising, spam, posts that reflect irresponsible practices, are off-topic, or contain vulgar language, posts that may violate the rights of others, or violate any social community's terms of use, may be removed. We also reserve the right to block users from posting content.
We love to see all your comments, photos and videos. By submitting or uploading your story, comment, photo or video, you are authorizing Evidencio to use, publish, and otherwise reproduce, modify and distribute Community Content with or without your name in perpetuity, worldwide in any and all Evidencio or Evidencio.com related media for any lawful purpose. These uses may include, but are not limited to, information, education, promotion or advertising of Evidencio.com or its products via the Internet, web sites, mobile apps, and social media. If individuals other than you appear in the photo or video, you must have permission to use the photo or video from the individuals.
2.5 CONTENT AND LIMITATIONS ON USE
You may print or download Content from the Site for your own personal, non-commercial, informational or scholarly use, provided that you keep intact all copyright and other proprietary notices.
You may not copy, display, distribute, modify, publish, reproduce, store, transmit, post, translate or create other derivative works from, or sell, rent or license all or any part of the Content, products or services obtained from the Site in any medium to anyone, except as otherwise expressly permitted under these Terms and Conditions, relevant license or subscription agreement or authorization by us.
You may not reverse engineer, disassemble, decompile or translate any software in the Content, or otherwise attempt to derive the source code of such software, except to the extent expressly permitted under applicable law, without our prior written permission. You may not engage in systematic retrieval of Content from the Site to create or compile, directly or indirectly, a collection, compilation, database or directory without our prior written permission.
Unless expressly authorized by us, you may not use any robots, spiders, crawlers or other automated downloading programs, algorithms or devices, or any similar or equivalent manual process, to: (i) continuously and automatically search, scrape, extract, deep link or index any Content; (ii) harvest personal information from the Site for purposes of sending unsolicited or unauthorized material; or (iii) cause disruption to the working of the Site or any other person's use of the Site. If the Site contains robot exclusion files or robot exclusion headers, you agree to honor them and not use any device, software or routine to bypass them. You may not attempt to gain unauthorized access to any portion or feature of the Site, any other systems or networks connected to the Site or to any Evidencio server, or any of the products or services provided on, accessed from or distributed through the Site. You may not probe, scan or test the vulnerability of the Site or any network connected to the Site or breach the security or authentication measures on the Site or any network connected to the Site.
3. PRIVACY POLICY
Evidencio is committed to maintaining your confidence and trust with respect to the privacy of the personal information we collect from you. Please read our privacy policy (https://www.evidencio.com/privacy-policy) carefully to understand how we collect, use and share your personal information, and what your rights are regarding personal information on our Site.
4. COPYRIGHT INFRINGEMENT NOTIFICATION
Evidencio is committed to complying with Dutch and international copyright law and to respond to claims of copyright infringement. Evidencio will promptly process and investigate notices of alleged infringement and will take appropriate actions.
Notifications of claimed copyright infringement should be sent to a Service Provider's Designated Agent. Notification must be submitted to the following Designated Agent for this site in the manner described below:
By Mail:
Evidencio
ATTN: Legal Department, Copyright Notices
Irenesingel 19, 7481GJ
Haaksbergen, the Netherlands
For your complaint to be valid, you must provide all of the following information when providing notice of the claimed copyright infringement:
- A physical or electronic signature of a person authorized to act on behalf of the copyright owner;
- Identification of the copyrighted work claimed to have been infringed;
- Identification of the material that is claimed to be infringing or to be the subject of the infringing activity, and that is to be removed or access to which is to be disabled, as well as information reasonably sufficient to permit Evidencio to locate the material;
- Information reasonably sufficient to permit Evidencio to contact the copyright owner, such as an address, telephone number, and, if available, an electronic mail address;
- A statement that you have a good faith belief that use of the material in the manner complained of is not authorized by the copyright owner, its agent, or law; and
- A statement that the information in the notification is accurate, and under penalty of perjury, that you are authorized to act on behalf of the copyright owner.
You should be aware that, claimants who make misrepresentations concerning copyright infringement may be liable for damages incurred as a result of the removal or blocking of the material, court costs, and attorneys' fees.
Last revised: June 15, 2021
Evidencio provides information, algorithms, calculators, equations and algorithms (tools) intended for use by healthcare professionals. Some of these tools have been certified as CE-medical devices. For such CE-marked content the ‘Official Legal Disclaimer for CE-marked content’ applies. All other content and tools provided by Evidencio are explicitly only covered by the ‘Official Legal Disclaimer for non CE-marked content’ both are available below.
Please note: your use of the websites, applications, apps or services provided by Evidencio is subject to our Terms & Conditions
Official Legal Disclaimer for CE-marked content
Evidencio provides certain CE-marked information, algorithms, calculators, equations and algorithms (tools) on any of its websites, applications, apps or services. These tools may only be used in accordance with the intended purpose that has been published with the respective CE-marked tool.
In general, and unless explicitly stated otherwise, CE-marked tools on Evidencio are only to be used by physicians in a clinical setting, and are not for patient use.
The CE-marked content on the platform is to be regarded as a specific set of tools, apart from the general platform content. Any available content, on any of the websites, applications, apps or services provided by Evidencio that is not clearly labeled as a CE-marked tool is explicitly not covered by this disclaimer for CE-marked content, the general Evidencio Disclaimer for non CE-marked content applies.
CE-marked tools may provide limited professional advice to the intended user(s). However, the intended user must exercise their own clinical judgment as to the information these tools provide.
Evidencio does not assume any liability or responsibility for damage or injury (including death) to you, other persons or property arising from any mis-use of any product, information, idea or instruction contained in the tools provided to you.
Last revised: May 20, 2020
Official Legal Disclaimer for non CE-marked content
Evidencio provides information, algorithms, calculators, equations and algorithms (tools) intended for educational, training and information purposes. These tools must therefore not be used to support medical decision making, or to provide medical or diagnostic services. Individuals who use the tools do so at their own risk. Individuals with any type of medical condition are specifically cautioned to seek professional medical advice before beginning any sort of health treatment. For medical concerns, including decisions about medications and other treatments, users should always consult their physician or other qualified healthcare professional.
The contents of the Evidencio Site, such as text, graphics and images are for informational purposes only. Evidencio does not recommend or endorse any specific tests, physicians, products, procedures, opinions, or other information that may be mentioned on the Site.
Evidencio explicitly does not warrant the accuracy of the information contained on this site.
Evidencio does not give medical advice, nor do we provide medical or diagnostic services. Medical information changes rapidly. Neither we nor our authors guarantee that the content covers all possible uses, directions, precautions, drug interactions, or adverse effects that may be associated with any therapeutic treatments.
Your reliance upon information and content obtained by you at or through this site is solely at your own risk. Neither we nor our authors assume any liability or responsibility for damage or injury (including death) to you, other persons or property arising from any use of any product, information, idea or instruction contained in the content or services provided to you.
Last revised: June 15, 2021
Evidencio is committed to maintaining your confidence and trust with respect to the privacy of the personal information we collect from you. Please read this privacy policy carefully to understand how we collect, use and share your personal information.
1. ABOUT OUR PRIVACY POLICY
This privacy policy describes how the personal information that is collected when you visit the Site, application or product that posts a link to this privacy policy ("Service"), will be used by Evidencio BV, the company that owns the Service ("Evidencio," "we," "us" or "our"). This policy may be supplemented by additional privacy terms, data processing agreements or notices set forth on certain areas of the Service, or explicitly agreed upon between Evidencio and yourself or your employer.
2. INFORMATION WE COLLECT
The Service collects information from you in two ways: directly from your input and automatically through the Service's technologies.
2.1 General
Evidencio acts as a Data Controller (as defined in Data Protection Legislation) regarding your 'Personal Data'. We process the data that is necessary for the execution of the Agreement between you and Evidencio BV. By accepting our ‘Terms & Conditions’ this Agreement is executed.
The data that is processed is the information that is necessary to provide you with our Services.
The Service is available for Users aged 18 and older. Our Terms of Use prohibit under aged Users from accessing the Service. We do not market our services to under aged individuals.
2.2 Information we collect automatically
The Service automatically collects information on how you use the Service, such as:
- The IP-address used to connect your computer to the internet is stored for 5 years, by our web server for security, maintenance and product improvement purposes;
- Computer, device, and connection information, such as browser type and version, operating system, mobile platform and other technical identifiers are collected in order to comply with e.g. medical device regulations;
- Service usage information such as URL click stream data, including date and time stamp, referring- and exit-URLs, search terms you used, and pages you visited or searched for on the Service.
We may use information that does not reveal your identity or permit direct association with any specific individual, such as browser and device information, anonymous usage data, and aggregated information, for any purpose, except where we are restricted by law. If we combine non-Personal Data with Personal Data, the combined information will be treated as Personal Data for as long as it remains combined.
We make very limited use of cookies. We use an ‘Evidencio Cookie’, to which you agree in our display a terms of service agreement modal, when you first visit the Service. This Evidencio Cookie is only used to set a unique session-ID, so that we can safely provide our Service, and your inputs don’t get mixed with information from other Users. You can control cookies through your browser's settings and other tools. However, if you block certain cookies, you may not be able to register, log in to the Services, access certain parts of the Services or make full use of the Services.
2.3 Information You Provide
The type of personal information you provide to us may vary, corresponding to the ‘role’ you have when interacting with the Service.
2.4 General Website and Service Use
When using the Service as a visitor without account, you may provide information to us by:
- Search terms you enter on the Service;
- Model parameter values that you specify in the Service in order to calculate a result;
- Your Name, Email address and Message, when using our contact form. Evidencio becomes the controller of this data, and processes this data on the basis of your consent to the processing.
This data is linked to the IP address that is collected automatically.
2.5 Registered Users
In order to access certain content and to make use of additional functionality and features of the Service, we ask you to register for an account by:
- completing and submitting a registration form; and
- accepting and agreeing to this ‘Privacy Policy’ and the ‘Terms & Conditions’.
In addition to the information you provide by your general use of the Service, you may provide us with:
-
Mandatory contact details:
- Username, Email Address, Occupation, Organizations
-
Optional contact details:
- First Name, Last Name, Address, Zip, City, Country, Website, Twitter-, Facebook-, LinkedIn-handle, a Profile Picture
-
Declarations
- Your declaration of having read, understood and agreed to our Terms of Use and Privacy Policy.
- Regarding the use of Medical Devices on the Service: your declaration of being a medical professional, and/or your declaration of adherence to the Medical Devices’ Intended Purpose.
2.6 Customers
Evidencio Customers, such as medical professionals, are also subject to the agreement as defined in the Paragraph ‘Registered Users’. They may be asked to provide additional information in order to fulfill the legal, administrative and financial obligations that need to be performed in the context of e.g. the use of Medical Devices as provided by the Service, such as:
- Payment information, as required by our Payment Providers;
- Your explicit warranty that you are qualified to use a specific medical device;
- Your input, time-of-use, calculated output, when using any Medical Device on the Service.
If you choose to sign in and use the Service by using a third party account (e.g. your Hospital account), the authentication of your login is handled by the third party and the Service will collect your name, email address, and any other information about your third-party account that you agree to share with us at the time you give permission for your account on the Service to be linked to your third party account.
2.7 Organizations
Evidencio Services can be purchased by organizations. In the contract between Evidencio and the Organization, the Organization can determine the purposes for which and the means by which personal data is processed. In this scenario the Organization is the data controller and Evidencio becomes the data processor. In this agreement the data necessary for the execution of the contract will be specified, but will likely consist of the data mentioned under points 2.5 and 2.6. Evidencio will only process data that is necessary for the execution of that Data Processing Agreement.
2.8 Job Applicants
If you apply for a job with us, for example, in response to a vacancy posted by us, but also if you send us an open application, you may provide us with your personal data (for example by sending us an email with your CV). Evidencio is a data controller of this data. We process this data on the basis of our legitimate interest to send you a reply.
- Any information you send us as part of a job application will be treated as personal information and will be destroyed once the job application process is concluded.
- The fact that you provide us with your job application and personal information does not mean we are obligated to provide you with any response whatsoever.
2.9 Email contact
It is Evidencio’s legitimate interest to process your name, email and message to reply to your support request, comments, questions or business inquiries, and customer support. This applies when you send an e-mail directly to Evidencio.
3. USE OF YOUR INFORMATION
We may use your Personal Data to:
- Provide the Service to you, by e.g. allowing access to, or delivery of our products or services, processing or fulfilling orders or transactions, or administering surveys or promotional programs;
- Respond to your requests, inquiries, comments, or concerns;
- Provide technical-, product-, and other support and help ensure safe and secure operation of the Service;
- Offer you customized content and individualized personalization of the Service to make it more relevant to your interests and needs;
- Enhance, evaluate, and improve the Service, its advertisements and promotional campaigns and our products and services and to develop new products and services;
- Identify and analyze usage trends, including for the purposes of research, audits, reporting and paying royalties and license fees to third-party content providers;
- Notify you about changes or updates to the Service and our other products and Services;
We do not make automated decisions based on your Personal Data.
4. DISCLOSURE OF YOUR INFORMATION
We may need to share a subset of your Personal Data with:
- Relevant entities, and representatives, for which we are acting as a partner, agent, licensee, or publisher, such as 3rd party IP-holders. These entities or representatives are always explicitly mentioned in relation to Service Content or within (Data Processing) Agreements governing your access to such Content;
- Applicable suppliers and service providers, including editors, reviewers, credit card processors, customer support, email service providers, but only in order to assist us with producing and delivering our products and Services, developing and operating our businesses, systems and applications, processing payments, providing customer support, communications, and for other purposes set forth in this privacy policy.
We also may need to disclose your Personal Data:
- To respond to or comply with any law, regulation, subpoena, court order or other legal obligation;
- To enforce and protect our rights and properties;
- To detect, investigate and help prevent security threats, fraud, loss, theft, misuse, unauthorized access, disclosure, alteration, or destruction if information;
- To protect the rights, property or safety of our Users, employees or others; and
The Service may let you post and share Personal Data, comments, materials and other content. Any information you disclose publicly may be collected and used by others, may be indexable by search engines, and might not be able to be removed. Please be careful when disclosing Personal Data in these public areas.
5. YOUR ACCESS TO YOUR INFORMATION
You have a right to be informed on Personal Data processed by the Service, a right to rectification/correction, erasure and restriction of processing. Upon request, you have the right to receive a structured, common and machine-readable format of the Personal Data you provided to us. We may need to request specific information from you to help us confirm your identity and ensure your right to access your Personal Data (or to exercise any of your other rights). This is a security measure to ensure that you are the data subject entitled to receive such Personal Data.
Access to your Personal Data will be provided free of charge. However, we may (in advance) charge a reasonable compensation should your request be clearly unfounded, repetitive, or excessive. At our sole discretion we may refuse to comply with your request in these circumstances.
As a registered User you can access your account information and make corrections or updates at any time. The accuracy of such information is solely your responsibility.
Where you have provided consent, you may withdraw it at any time, without affecting the lawfulness of the processing that was carried out prior to withdrawing it. Whenever you withdraw consent, you acknowledge and accept that this may have a negative influence on the scope and quality of the Service. We will endeavor to fulfill your request within 30 days but some Personal Data may persist in backup copies for a certain period of time and may be retained as necessary for legitimate business purposes or to comply with our legal obligations. You agree that Evidencio BV shall not be held liable regarding any loss and/or damage to your Personal Data if you choose to withdraw consent.
To exercise any of the rights mentioned in this Privacy Policy and/or in the event of questions or comments relating to the use of your Personal Data, you may contact Evidencio at: privacy@evidencio.com
You have the right to file a complaint with the data protection authority in your jurisdiction. However, we would very much appreciate it if you would file your complaint with us before going to a data protection authority.
6. DATA RETENTION
Evidencio acts as a Data Controller regarding your Personal Data. As such, we have defined data retention policies regarding your Personal Data.
Data retention:
- Information you provide as part of your User profile will be stored as long as your profile exists. In part some information may be retained longer due to legal requirements (e.g. due to legislation medical device use)
- Information you provide as part of your Service Subscriptions (e.g. payment, tax, or company information) we are required by law to retain for 10 years.
- Information we collect automatically: 5 years.
- In case you use the Service as part of your employment at an organization that has an Evidencio Subscription with associated Data Processing Agreement in place. Particular details on data retention regarding tour use of the Service may be specified in the respective Data Processing Agreement.
- Information you have given us for contacting you, including e-mail address and messages, regarding any medical device, needs to be retained up to 10 years after the last medical device has been placed on the market for safety reasons.
You should be aware that we may retain certain Personal Data to comply with legal obligations, resolve disputes and enforce our agreements.
7. DATA SECURITY
Evidencio has taken every reasonable precaution to safeguard your Personal Data against loss, theft, misuse, unauthorized access, disclosure, alteration, and destruction through the use of appropriate administrative, physical and technical security measures.
Our company and Services have been ISO27001 and NEN7510 certified.
As part of our obligations under these information security certifications our Service is periodically scanned for security holes and known vulnerabilities in order to make your visit to our site as safe as possible. Your Personal Data is contained behind secured networks and is only accessible by a limited number of persons who have special access rights to such systems, and are required to keep the information confidential.
Personal Data and usage data is stored as long as is necessary for the purpose(s) for which we originally collected it. We may also retain information as required by law.
8. CROSS-BORDER TRANSFER OF INFORMATION
Evidencio’s Service is hosted on Amazon AWS cloud infrastructure. We currently use AWS Services located in Ireland and Germany. Your Personal Data may be transferred to either Ireland or Germany for processing. By using the Service, you consent to the transfer of information to these countries which may be outside of your country of residence, and which may have different Personal Data protection rules than in your country.
9. CHANGES TO OUR PRIVACY POLICY
We may change this privacy policy from time to time, at our sole discretion. Any changes will be posted on this page with an updated revision date.
10. LINKS TO THIRD PARTY PRODUCTS & SERVICES
The Service may, at our discretion, include or offer third-party products or services. These third-party products or services may have separate and independent privacy policies. We, therefore, have no responsibility or liability for the content and activities of these linked products or services. Nonetheless, as we endeavor to protect the integrity of our Service, we welcome any feedback regarding these third-party products and services.
11. COMPLIANCE WITH LOCAL LAWS
11.1 EU General Data Protection Regulation (“GDPR”)
We carry out all data control and processing operations in strict compliance with the GDPR. We use a limited number of external service providers that are trusted and meet high data protection and security standards for certain tasks such as technical data analysis, processing and/or storage offerings. We only share information with them that is required for the services offered, and we contractually bind them to keep any information we share confidential. We will not pass your data on to third parties without your express consent unless we are obliged to do so by statutory law or an instruction from a public authority or court.
11.2 California Online Privacy Protection Act
- Users can visit our site anonymously. This privacy policy is available through a clear link on every page on our site. Our Privacy Policy link includes the word 'Privacy' and can be easily be found on any page on the site. Users that opt to create an account on our site will be notified of any privacy policy changes when they login to their account.
- We honor “do not track” signals and do not track, plant cookies (other than a functionally required session cookie), or use advertising when a Do Not Track (DNT) browser mechanism is in place.
Should a data breach occur;
- We will notify the Users via email within 7 business days.
- We also agree to the Individual Redress Principle.
- We do not market to children under 13.
- Please note that we allow third-party behavioural tracking to improve our Service and our user experience.
11.3 CAN-SPAM ActPrivacy Protection Act
- If at any time you would like to unsubscribe from receiving future emails from Us, you can email us at privacy@evidencio.com and we will promptly remove you from ALL correspondence.
12. CONTACT
If you have any questions, comments or requests regarding this privacy policy or our processing of your information, please contact:
Evidencio BV
Attn: Privacy Officer
Irenesingel 19
7481 GJ
Haaksbergen
the Netherlands
privacy@evidencio.com
Last revised: June 09th, 2023
Login
Sign Up
With an Evidencio Community account you can:
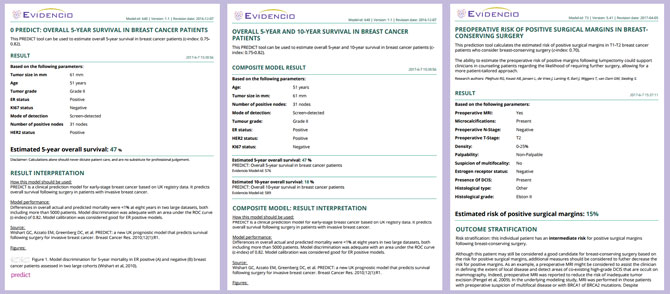
- Create and publish your own prediction algorithms.
- Share your prediction algorithms with your colleagues, research group, organization or the world.
- Review and provide feedback on algorithms that have been shared with you.
- Validate your algorithms and validate algorithms from other users.
- Find algorithms based on Title, Keyword, Author, Institute, or MeSH classification.
- Use and save prediction algorithms and their data.
- Use patient specific protocols and guidelines based on sequential algorithms and decision trees.
- Stay up-to-date with new algorithms in your field as they are published.
- Create your own lists of favorite algorithms and topics.
A personal Evidencio account is free, with no strings attached!
Join us and help create clarity, transparency, and efficiency in the creation, validation, and use of medical prediction algorithms.
.png)
.png)